
When Barb Clark’s two-year-old daughter first started stealing, she wasn’t worried. Many toddlers steal, and then they learn that stealing isn’t okay. But fast forward four years and the stealing hadn’t stopped.
Barb—an adoptive parent and specialist with Families Rising—and her husband tried everything, but many of their strategies were focused on consequences. The stealing saga culminated in one fateful day. Barb and her husband sat their daughter down and told her that if she stole again, they would throw away her most prized possession: her yellow blankie. They went to bed feeling like they had cracked the code: she would never steal again. But the next day? The stealing continued, and the parents threw away that blankie.
But that consequence did not work. She continued to steal, and now she also couldn’t sleep. Over a decade later, their daughter still looks back at that as a painful memory.
She and her parents were eventually able to get the right guidance and support. But to this day, Barb regrets throwing that blankie away. And it sent her on a journey to understand how to be a trauma-responsive parent.
“I wish I had known what I know now back when we first were starting our family, so I’m really passionate about getting this information out,” Barb explains.
What is trauma-responsive parenting?
Trauma-responsive parenting:
- Focuses first and foremost on the relationship you have with your child.
- Does not shame or blame the child.
- Understands what is happening in the brain to cause behavior challenges.
- Is not instinctive or intuitive. This is a hard one because we are all used to a certain parenting style. Switching from traditional parenting methods, like using consequences and control, is hard.
- Acknowledges a child’s developmental age. A child’s chronological age and developmental age aren’t always the same, especially for kids with trauma histories.
Trauma-responsive parenting should be used for children with any type of trauma history, whether it is in-utero trauma, like a fetal alcohol spectrum disorder, or out-of-utero trauma. “And honestly, I think we should be using these strategies for all children, ones that haven’t experienced trauma even,” Barb said.
Is consequence-based parenting really that bad?
Most parents, and perhaps you might relate to this, instinctively go to consequence-based parenting methods. It’s how almost all of us were parented, too. But, these methods:
- Often cause further trauma to the child.
- Slow down and often stop attachment. If all we’re doing with a child is giving consequence after consequence, it is harder for a child to develop attachments with their caregivers.
- Can make a child feel unsafe. Having things taken away is something many children might have experienced before they came into their foster or adoptive family. And it doesn’t feel safe to constantly have someone taking things from you.
- Increase anxiety. This is one of the most important things to think about. Kids don’t learn well when they’re anxious. Plus, a lot of behaviors are rooted in anxiety. When kids are in trouble, they feel a lot of anxiety in that moment. While we’re having the talk for the millionth time about a behavior, children are not able to store and process that information while they’re feeling anxious.
If you’re convinced that trauma-responsive parenting might be a good approach for your family, you may be feeling guilty for using different styles in the past. Barb shares that it did not feel good when she realized she was part of the problem and was impacting her relationship with her daughter. But remember that you’re human. It’s okay to realize some of your past parenting approaches might not have worked and to try these trauma-responsive ones moving forward.
Here’s how to embrace this highly effective parenting style
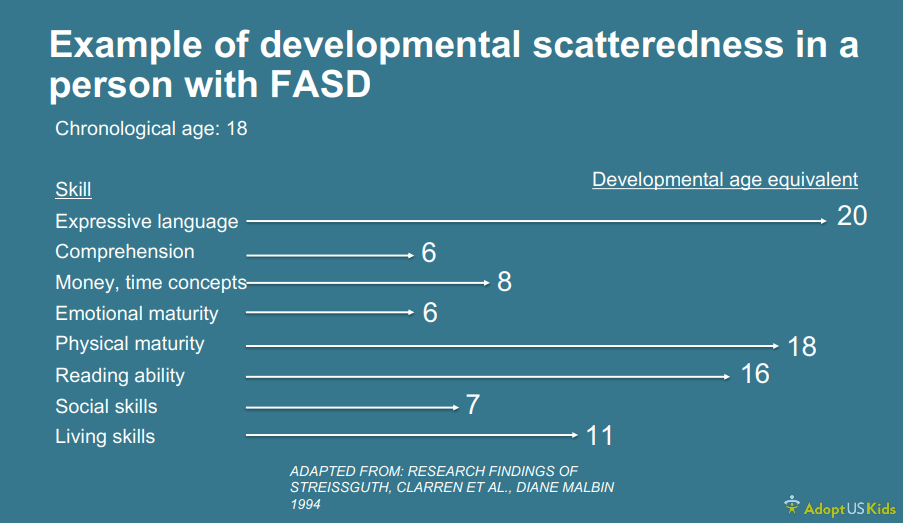
First, accept that your child’s brain may be different, and brain age does not always match birth age. You should learn about your child’s brain age across different skills. For example, a child with a fetal alcohol spectrum disorder (FASD) may be 18 years old. Their developmental age might be 20 years old for expressive language and 6 years old for comprehension, as the image below shows.
If applicable, accept that brain injury has caused a disability. Just like physical disabilities, behavioral disabilities exist. And even though you can’t see neurodiversity and other brain differences, they still impact everyday life. “I recommend families start learning about the brain and start teaching their kids about the brain,” Barb encourages.
It will also help to accept the reality of your family’s circumstances. It’s not lowering expectations—it’s changing them. Grieve your losses and help your child grieve theirs, too. When kids lose out on some of the experiences we would hope and want them to have, we should help them to grieve those losses.
Finally, it can be helpful for parents to join support groups. This way, you can hear from real families about how trauma-responsive parenting has worked for them.
Barb shares, “It wasn’t until I started to meet and connect with other parents who were parenting similar kids that I started to learn that I was a part of the problem and that I needed to start doing things differently. It brought me out of the dark hole that I was in. We were in major crisis and not happy and our household was this toxic environment of chaos. When we finally got the right support and connections, things started to change. It takes a while to change, but it’s so worth it.”
Keep these additional tips in mind:
- If you feel hesitant, try trauma-responsive parenting for just 6 months.
- Be patient.
- Give yourself grace.
- Apologize when you make mistakes.
- Forgive, forget, and move forward.
Keep learning about trauma
- Changing our approach when our children can’t change
- Helping a child through a crisis
- Is it lying or confabulation—and how should I respond?
- Understanding adverse childhood experiences and what you can do to help
This article is based on a webinar that Barb Clark delivered for AdoptUSKids. We thank Barb for granting us permission to share her insights.